
@ShahidNShah

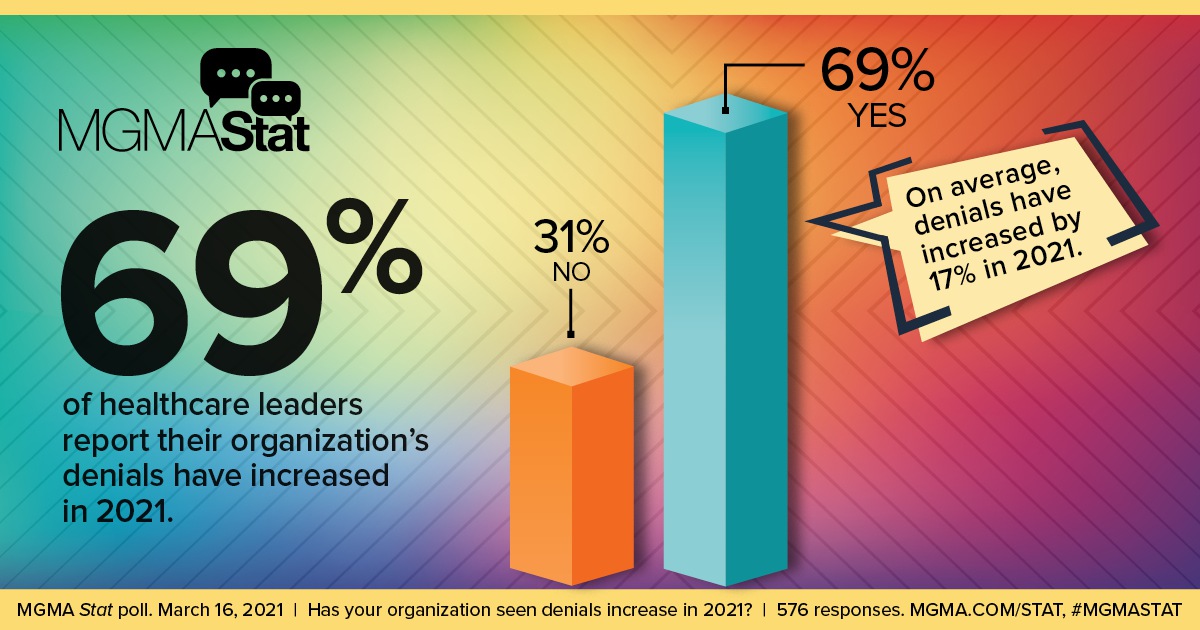
The good news for practices is that most denials can be avoided if the above challenges are addressed. The bad news is that if claims are not addressed, the average cost to rework a claim is $25.20, which quickly adds up.
That’s why it’s important for front office staff to be trained to inquire about additional coverage. They should also confirm eligibility through the use of technology, prior to service, at the time of service, and before submitting a claim. Registration data should be examined for accuracy, completeness, and consistency, and any mistakes should be remedied as part of the normal workflow to avert downstream denials.
With medical coding, staff should focus on the accuracy of discharge status coding and admit/discharge rates and also confirm that the chargemaster is up to date and accurate.
Continue reading at mgma.com
Providers care deeply about their patients and delivering the best care possible to them. Patients want to be listened to, understood, and comforted. Active engagement for patients could be, for …
Connecting innovation decision makers to authoritative information, institutions, people and insights.
Medigy accurately delivers healthcare and technology information, news and insight from around the world.
Medigy surfaces the world's best crowdsourced health tech offerings with social interactions and peer reviews.
© 2025 Netspective Foundation, Inc. All Rights Reserved.
Built on Jul 18, 2025 at 12:24pm